THE prevention of COVID-19 by taking Vitamin C fruits, using herbs and steaming to prevent contraction is good but when a patient is very sick and experiencing ‘sot win’ or shortness of breath, it is best to seek medical attention at a hospital.
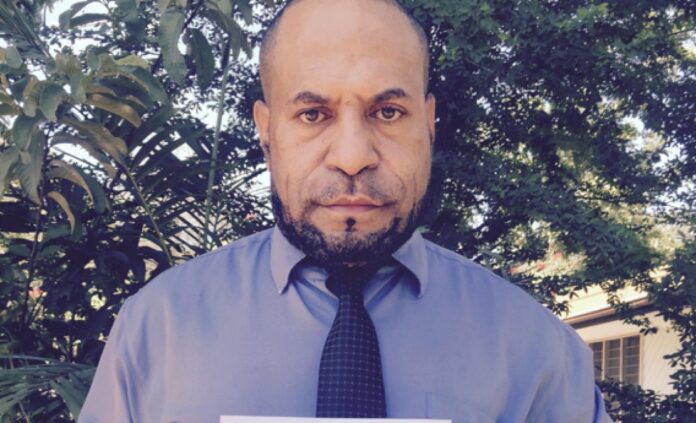
The head of Port Moresby General Hospital’s Emergency Division, Dr Sam Yockopua pointed this out at a recently concluded UPNG SRC Panel Discussion on COVID-19.
Dr Yockopua said it is best to seek medical attention at the hospital where ventilators are available when very sick patients are suffering from shortness of breath.
He was one of the five panelists who were present to discuss the state of COVID-19 in Papua New Guinea and the AstraZeneca vaccine at UPNG’s Main Lecture Theatre last week.
During the panel discussion, questions were posed by several students as to why there is an increase in the number of Covid-19 cases and associated deaths as a result of something they’ve never experienced before.
Dr Yockopua explained how the alarming rise in the COVID-19 death toll as a result of the virus targeting patients with underlying chronic diseases and associated deaths.
He highlighted that various at-home remedies that have been popularized through social media, such as steaming and consumption of fruits containing vitamin C, can only prevent the spread of the virus and the worsening of its symptoms.
“But if the patient is very sick and his or her oxygen level is low this is dangerous”.
By sharing a case of an unnamed patient who passed away from low oxygen levels in the blood, Dr Yockopua explained that even with the traditional or routine prescription of drugs and at-home remedies, this symptom of the coronavirus has been a reoccurring passage to death this year.
“If you can do home remedies that’s fine but once you feel sick or particularly experiencing sot win, you might have an oxygen saturation of 75% -80% and if you continue to stay at home, you can die while sleeping. So its better you come to the hospital where we can measure the oxygen levels in your blood to avoid this,” the doctor said.

He added that this becomes an even bigger issue, as there are a limited number of ventilators currently available for patients coming in with difficulty breathing, one of the many crucial pieces of equipment the dire and underfunded PNG health system is in need of.
“It comes as no surprise that the numbers have gone up after one year of operating with already limited resources allocated to the pandemic,” Dr Yockopua said.
The COVID-19 death toll has reached 68, while the total number of cases sits at 8,342. While these numbers represent patients with varying medical conditions, some with underlying chronic illnesses such as diabetes and high blood pressure, as well as others who are perfectly healthy, those with pre-existing conditions are at a higher risk of death.
Dr Yockopua stressed that the COVID-19 virus, once contracted by people in this state, increases the rate of deterioration to their already distressed medical state and this ultimately leads to death.
“The analogy is like having a tree that is eaten by beetles overtime and even with strong winds it keeps standing until someone pushes it and it falls, and that pushing it off is COVID.”
This catalytic effect of the coronavirus has led to the current steady increase in deaths this year, whereby those cases in Port Moresby have been determined and reported by Dr Yockopua and his frontline clinical team. Compared to last year’s statistics and the occasional post on social media by non-medical professionals, the public have been misled to question why these deaths have been declared as COVID deaths, particularly of deceased patients who have known long-term chronic illnesses. When given this issue to address, Dr Yockopua explained candidly the process of determining the cause of death.
“When we clinically suspect that the cause of death was due to COVID, we do a swab and then send it to the labs while the body is in layout. We get the lab guys to run the tests for us and we don’t issue any documents, we just fill in a DOA (death on arrival) form. It’s a preliminary form to document the death and then we write down ‘COVID test pending’ and then we wait for the results to come back. Usually the POMGEN Laboratory takes about three hours, or sometimes we can get them to do it in two hours. If it is negative, that the cause of death is due to something else, but if it is positive, we look at the records of the underlying conditions and then we associate the death as part of COVID.”
This explanation establishes that the deaths reportedly caused by the COVID-19 virus are in association, and therefore their DOA forms will note this as well as the pre-existing conditions. This association, as Dr Yockopua puts it, automatically counts the deceased as a death in the collation of COVID-19 statistics in Papua New Guinea.